FAQs
If you have any additional questions or would like to receive more information, please contact our OMPT Fellowship Director, Daniel Maddox at dmaddox@urpt.com
Eligible applicants must….
- have graduated from a CAPTE-accredited entry-level physical therapy program.
- be a current full-time or part-time employee of the Upstream Rehab Partners or must otherwise sign an offer letter for full-time or part-time employment with Upstream Rehab Partners upon provisional acceptance and prior to matriculation.
- possess a current state license to practice physical therapy within the United States.
- possess at least 2 years of experience practicing in an outpatient orthopaedic setting AND meet one of the following additional criteria:
- a.) has obtained an ABPTS specialist certification prior to matriculation (NOTE: Those awaiting ABPTS specialty exam results are eligible to apply.), OR…
- b.) has graduated from an ABPTRFE-accredited clinical residency program prior to matriculation.
- be AAOMPT members in good standing – or must otherwise join or reinstate membership upon provisional acceptance and before matriculation.
The program is designed to be completed in approximately 24 months, beginning in January of one year and culminating in December of the following year. This is the standard program length and structure.
However, the program also offers an 18-month “accelerated option” that would begin in the summer of one year and culminate in December of the following year. Those matriculating under the accelerated option would join with the cohort that had started in January and subsequently progress through program as members of a unified cohort.
The same content and curriculum are delivered under either option. However, the accelerated option results in a more compressed curriculum – and thus a more demanding schedule. While not a hard requirement, it is suggested that those who wish to pursue the accelerated option have completed an orthopaedic residency previously.
We welcome applications from both inside and outside of Upstream Rehab Partners. As a fellow-in-training, you must be employed by Upstream Rehab Partners before matriculation into the program. We are happy to assist in that process.
The program can be completed from the vast majority of the clinics throughout the company. The only potential obstacle to participation would be based on geographic proximity to a qualified mentor. However, we do have qualified mentors located throughout the country, and thus far we have never had to turn any candidate away due to difficulty with mentoring logistics. With that said, identification of potential mentors and coordination of mentoring logistics including travel as necessary will be considered during the admissions process and discussed with the candidate and all relevant stakeholders prior to official matriculation.
Qualified applicants participate in a video conference interview with the program director and select faculty and/or past or present program participants.
Yes. Fellows-in-training are full-time or part-time employees of Upstream Rehabilitation and earn a full salary and receive benefits consistent with their status as full-time or part-time employees.
The overall cost of the program is $15,000 – which includes all course materials, weekend lab courses, faculty costs, online cohort collaboration, fellowship-related travel, and assistance with mentoring hours. Two-thirds of the cost ($10,000) may be covered by Upstream Rehabilitation in exchange for a post-graduation commitment – leaving the fellow-in-training with a responsibility of $5,000. This $5,000 may be paid up front, or the fellow-in-training may opt for an interest-free loan in the form of an automated payroll deduction over the duration of the chosen track (18 or 24 months).
Yes. The URI Fellowship in Orthopaedic Manual Physical Therapy is dually accredited by both the Accreditation Council on Orthopaedic Manual Physical Therapy Education (ACOMPTE) and the American Board of Physical Therapy Residency and Fellowship Education (ABPTRFE).
The program accepts a maximum of 6-8 applicants per annual cohort – inclusive of those who begin in January AND those joining in the summer under the accelerated option.
Graduates are immediately eligible to become a Fellow of the American Academy of Orthopaedic Manual Physical Therapists (FAAOMPT).
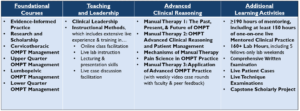
The fellowship curriculum includes four primary components:
- Mentorship and Clinical Practice, including:
- 150 hours of mentoring with a FAAOMPT
- 160+ hands-on lab hours
- Written and video case presentations with ensuing asynchronous and synchronous discussions
- Didactic coursework via online, blended, and on-site components
- Educational development via guided TA roles and assignments related to presentation and content development.
- Capstone Projects to include two written final examinations, a live technique examination, and a scholarly project.
The following is an outline of the various didactic components and capstone requirements:
Each fellow-in-training will complete 150 hours of 1-on-1, mentored clinical practice. 150 hours of mentoring must be completed under the guidance of a FAAOMPT, including at least 75 hours of 1-on-1, on-site, mentored clinical practice. The mentoring completed under a FAAOMPT may be supplemented with mentoring under an approved mentor who has undergone fellowship training in another related area of advanced sub-specialty – such as pain science, movement science, or spine care. A primary mentor, and typically a secondary mentor, will be assigned upon matriculation. The logistics of mentored clinical practice will vary according to each participant’s individual situation. For example, participants whose mentor is located in the same clinic or town may choose to set aside several hours every week for mentored clinical practice, while others whose mentors are located further away may choose to do several longer blocks (i.e. several days in a row or a full week) of mentored clinical practice scattered throughout the curriculum. The logistics of mentoring will depend on what is best for each individual fellow-in-training and his or her clinical situation, and will be planned in consultation with the participant’s operational supervisor (i.e. clinic director, area director, etc.) and URI mentoring coordinator.
Mentoring is always a structured experience in regards to each session, but the venue may be flexible. A core value for URI is adaptability and we therefore allow mentoring to occur at the fellow-in-training’s clinic, the mentor’s clinic, or a combination of both locations (most common). There are options for a portion of hours to be completed virtually as well.
Just what it sounds like! We offer the majority of our didactic coursework via multiple distance technologies to allow for unique opportunities and experiences. We combine this with 10 live weekend labs and mentored clinical practice to advance your practice via hands-on learning and feedback from our expert faculty.
Utilizing a blended learning format provides a level of convenience and accessibility to the fellow-in-training – as it allows him/her to complete the program from almost anywhere in the United States and eliminates the need to relocate to pursue a fellowship experience. In addition, it allows the program to provide a collaborative experience from all of our highly qualified faculty regardless of location, resulting in a high-quality and consistent experience for all fellows-in-training.
There are so many reasons!
- Mastery of advanced manual assessment and treatment techniques
- Development of highly advanced clinical reasoning processes
- Proficiency in critical appraisal and integration of research into evidence-informed practice
- Training and real-world experience in education via a variety of mediums
- Guided experience in scholarly productivity (ie…research, conference presentation, etc.)
- Improved outcomes! Published research studies have shown that fellowship-trained clinicians achieve significantly greater clinical outcomes than their non-fellowship-trained peers. In addition, our own internal data clearly demonstrates that our graduates achieve significantly better outcomes and improved operational proficiency vs non-fellowship-trained clinicians within Upstream Rehab Partners clinics.